Varicose Ulcers
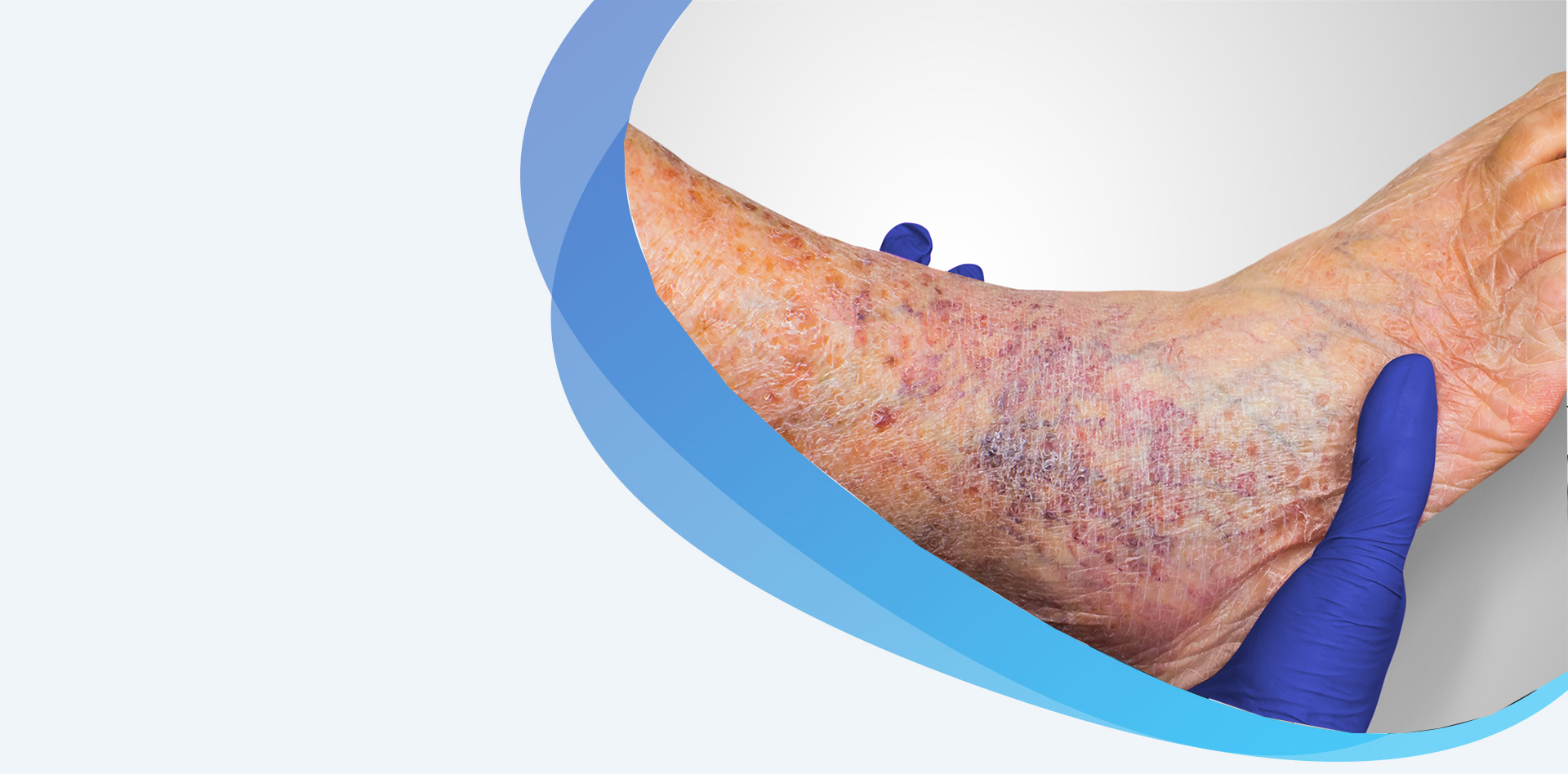
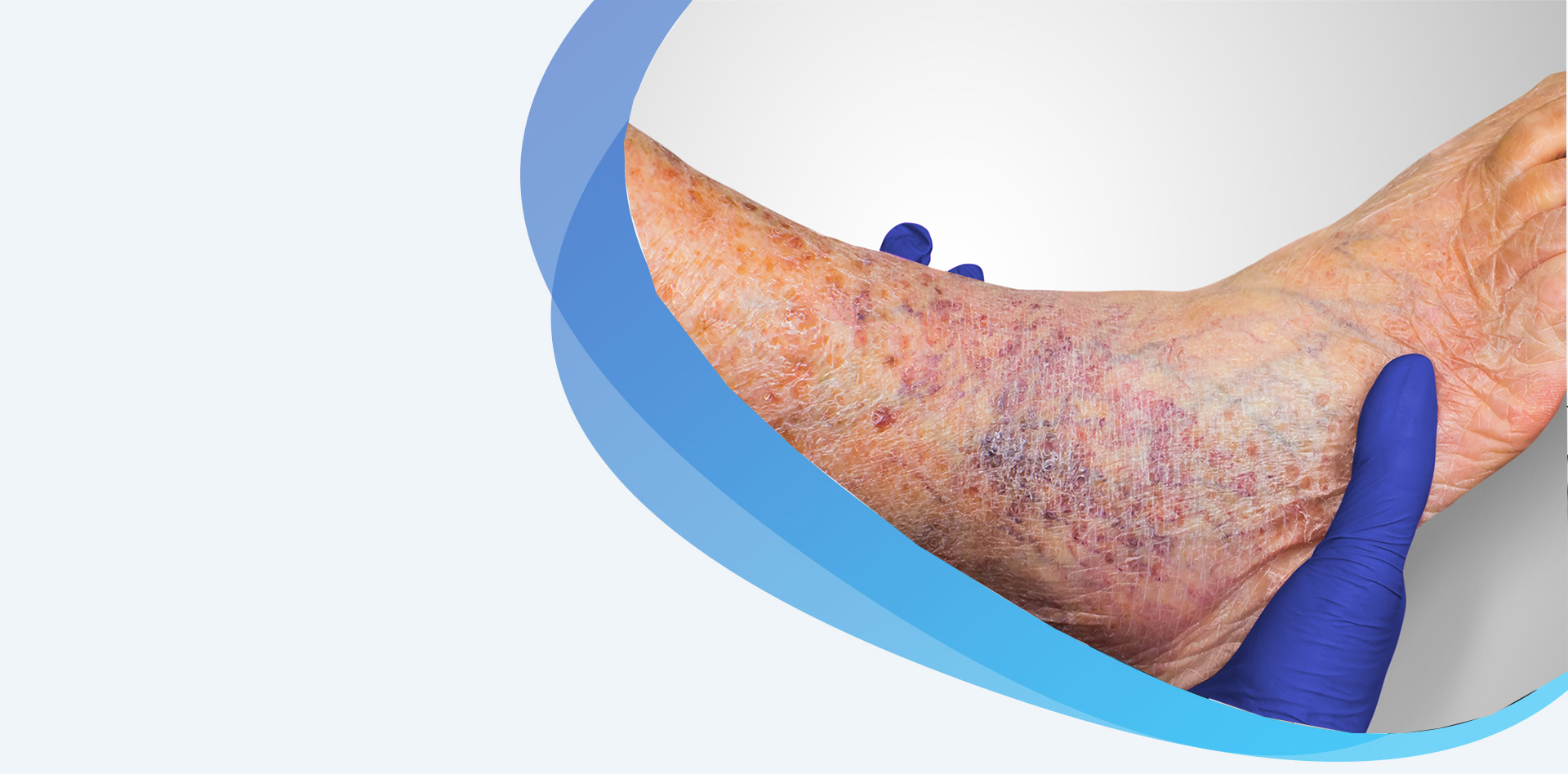
A venous ulcer, sometimes called a varicose ulcer, is a leg wound that happens when the leg veins don’t circulate blood back toward the heart. Blood can back up in the veins, building up pressure on the skin, which can cause an open sore to form.
Venous ulcers usually form on the sides of the lower leg, above the ankle and below the calf. They are slow to heal and often return. Without proper treatment, they can become larger and cause additional leg problems.
Venous ulcer (varicose ulcer) symptoms include:
If a venous ulcer is suspected, your physician will do a complete physical, including a check of your blood pressure in your arm and your ankle. Accurate diagnosis is the foundation of good ulcer care. The diagnosis is typically made based on the description of how the ulcer began and physical exam findings. Additional tests may include:
Ankle brachial index test: During this test, blood pressure cuffs are placed on the arms and ankles. A handheld ultrasound device or ‘Doppler’ is used to listen to the blood flow and measure the blood pressure. This helps doctors understand if there is a decreased blood flow to the lower legs and feet.
Ultrasound: An ultrasound device can measure blood pressure on various points of your arm or leg, which will help the physician determine if you have any blockages and how quickly blood flows through your arteries in the lower leg.
In addition, ulcers should be assessed for infection. A culture of the wound may be used to determine if antibiotics are needed. In addition, these tests may also be used:
Imaging tests: X-rays, magnetic resonance imaging (MRI), or bone scans can help identify bone infection and help determine whether surgery is needed to remove all of the infection.

Venous ulcers have several causes, typically lifestyle factors or results. The following can lead to venous ulcers:
Risk factors that can contribute to venous ulcers include:
While you cannot prevent certain risks for venous ulcers, you can take steps to lower your chances of developing the condition:
Don’t smoke: If you do smoke, ask your physician about programs and strategies that can help you quit.
Control high blood pressure and cholesterol: Eat a healthy diet, exercise and take medications as prescribed.
Manage your diabetes: If you have diabetes, keep blood sugar levels under tight control.
Maintain a healthy weight: Eat a low-fat, low-sugar diet high in fruits and vegetables and exercise regularly to keep your weight stable.
Wear compression stockings: People with chronic venous insufficiency should wear compression stockings daily.
Avoid sitting or standing for long periods of time: Take regular breaks to walk and stretch.

With proper treatment, most venous ulcers heal within three to four months.
Treatment for venous ulcers includes controlling the high pressure in the leg veins and treating the ulcer.
Controlling Pressure in the Leg Veins
Controlling swelling is essential for patients with venous ulcers. Leg elevation, with the feet at or above the level of the heart, several times throughout the day and while sleeping, can help reduce swelling. Compression wraps or bandages are often applied to the legs. These can be changed as often as multiple times a day or as infrequently as once a week, depending on the amount of fluid draining from the ulcer. Once the ulcer is smaller or nearly healed, elastic compression stockings may be recommended. Compression stockings are sized to fit the legs and are typically put on in the morning and worn throughout the day. A venous pump may be prescribed for patients with severe swelling.
Treating the Ulcer
The first step in treating a venous ulcer is to remove any dead tissue around the sore and then to apply a special dressing to encourage healing. The dressing will need to be changed about once a week. Sometimes a compression stocking will be worn over top of the dressing. The first few weeks with a compression bandage on an ulcer are usually painful. Your doctor will prescribe and appropriate pain reliever. As the ulcer heals, the pain will lessen.
Surgery
Patients who have developed poorly healing sores in relation to their varicose veins require more advanced wound care and treatments. New varicose vein treatment options are minimally invasive, require minimal anesthesia and are safely performed in outpatient surgery centers or doctors’ offices. Treatment choices depend on the vein groups that are causing symptoms and can include:
Lifestyle Changes
Many patients with venous ulcers or who are at risk of developing a venous ulcer can reduce symptoms and lower their risk by quitting smoking, increasing exercise and eating a healthy, low-fat, low-sodium diet, and avoiding sitting and standing for long periods of time.
A venous ulcer can lead to a variety of serious health problems, including:
Loss of mobility: A venous ulcer can be painful and that can limit activity, which will make the condition worse.
Infection: Venous ulcers can easily become infected. If the infection is not treated, it can lead to blood poisoning or an infection of the bone.

The Vein & Artery Clinic is known for advanced, superior care in the diagnosis, management and treatment of patients with venous ulcers. Treatment of venous ulcers, also known as a varicose ulcer, can be complicated and we has a team of super-specialist vascular surgeons who specialize in the management of arterial and venous pathology. This includes medical management, expert diagnosis, minimal invasive treatments (often in the office), and wound care.
You will appreciate timely appointments and respectful attention to your concerns, all in a positive and friendly atmosphere. Here, you have access to the region’s most comprehensive, multidisciplinary team of specialists and innovative therapies, including many available only through specialized clinical trials. In every way, we work to demonstrate the utmost excellent care to those who trust us with their health.