An aortic dissection is a tear in the lining of the aorta that creates two blood flow channels. One channel is called the true lumen, which feeds blood to most of the important branches of the aorta and is surrounded by the normal aortic lining. The second channel is called the false lumen, which may only feed a few (if any) important branches.
Aortic dissection is a very complicated condition. Untreated, an aortic dissection can lead to death.
A dissection that involves the ascending aorta almost always requires emergency open-heart surgery to repair the vessel and prevent death. ONLY OPEN SURGERY TREATMENTS for distal dissections occurring beyond the left subclavian artery (feeds the left arm) are described here.
Treatment of an aortic dissection may be needed if:
- Your aorta begins to dilate rapidly.
- After your blood pressure and heart rate are well controlled, you experience sharp pain or a tearing sensation in your chest and back.
- Your aorta leaks or ruptures, in which case emergency treatment is in order.
- Important branches of your aorta become distressed or dysfunctional.
- Over many years your aorta dilates and a thoracic or thoracoabdominal aortic aneurysm forms.
Whether endovascular or open surgery treatment is best for you depends on multiple factors, including the anatomy of the dissection, your age and health condition.
1) Treatment is first given is to control your blood pressure and heart rate, usually in the emergency room.
2) A CT angiogram is used to determine the location and extent of the dissection, and to evaluate what part of the aorta and which aortic branches may be involved.
3) If open surgery treatment is appropriate, one of the two procedures below will likely be recommended.
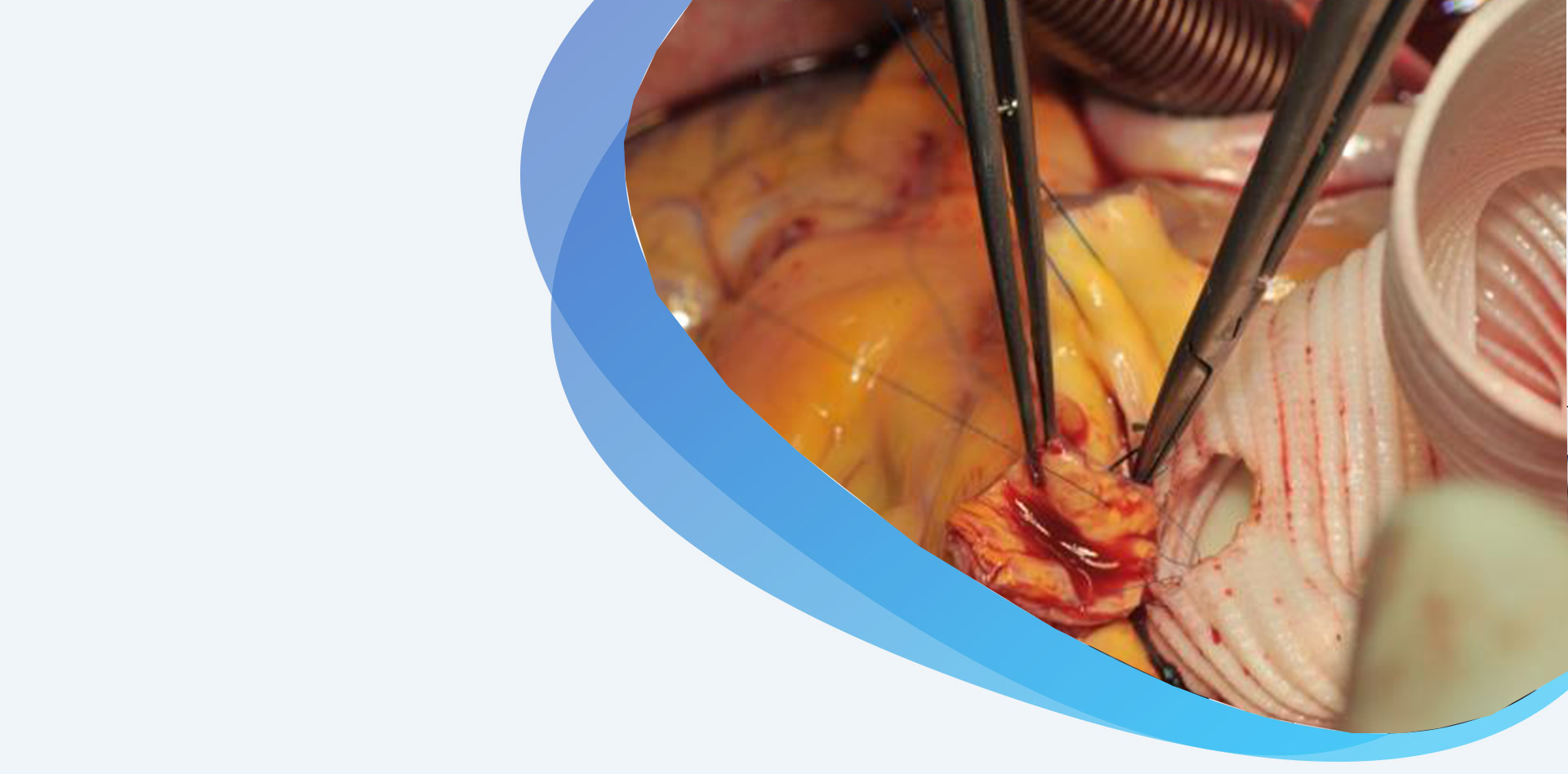
OPEN SURGERY FENESTRATION
This procedure is done to improve blood flow to the arteries that feed the abdominal organs and kidneys, and sometimes the pelvis and legs. The operation entails removing the dissection flap from the aorta and possibly replacing a portion of the aorta.
- You are given general anesthesia.
- Once you are comfortable, you are positioned so that you are lying on your right side. An incision is made along your left side that can extend from your chest to your abdomen.
- Your ribs are spread. Your vascular surgeon moves aside several organs (lungs, colon, spleen, pancreas) in order to reach the part of your aorta that needs to be fixed.
- Once the aorta is accessible, medication is given to thin your blood and reduce your blood pressure.
- The aorta and major branches feeding the abdominal organs and kidneys are clamped. The aorta is then opened and the dissection flap is removed. If the dissection also affects the aortic branches, these areas are repaired.
- Next, the damaged portion of the aorta is repaired. Once repair is complete, clamps are removed to restore blood flow. Flow in the branch vessels is tested using a Doppler ultrasound.
- If circulation to the legs and pelvis needs improvement, the aorta below the kidney arteries is clamped and opened. Small bleeding branches are over-sewn. To promote blood flow the vascular surgeon creates small holes in the areas around the clamp and removes the dissection flap. The damaged portion of the aorta is then replaced with a cloth tube that is sewn to the open ends of the aorta.
- Once all necessary work is complete, blood thinner medication is reversed. Your organs are checked and wounds are closed.
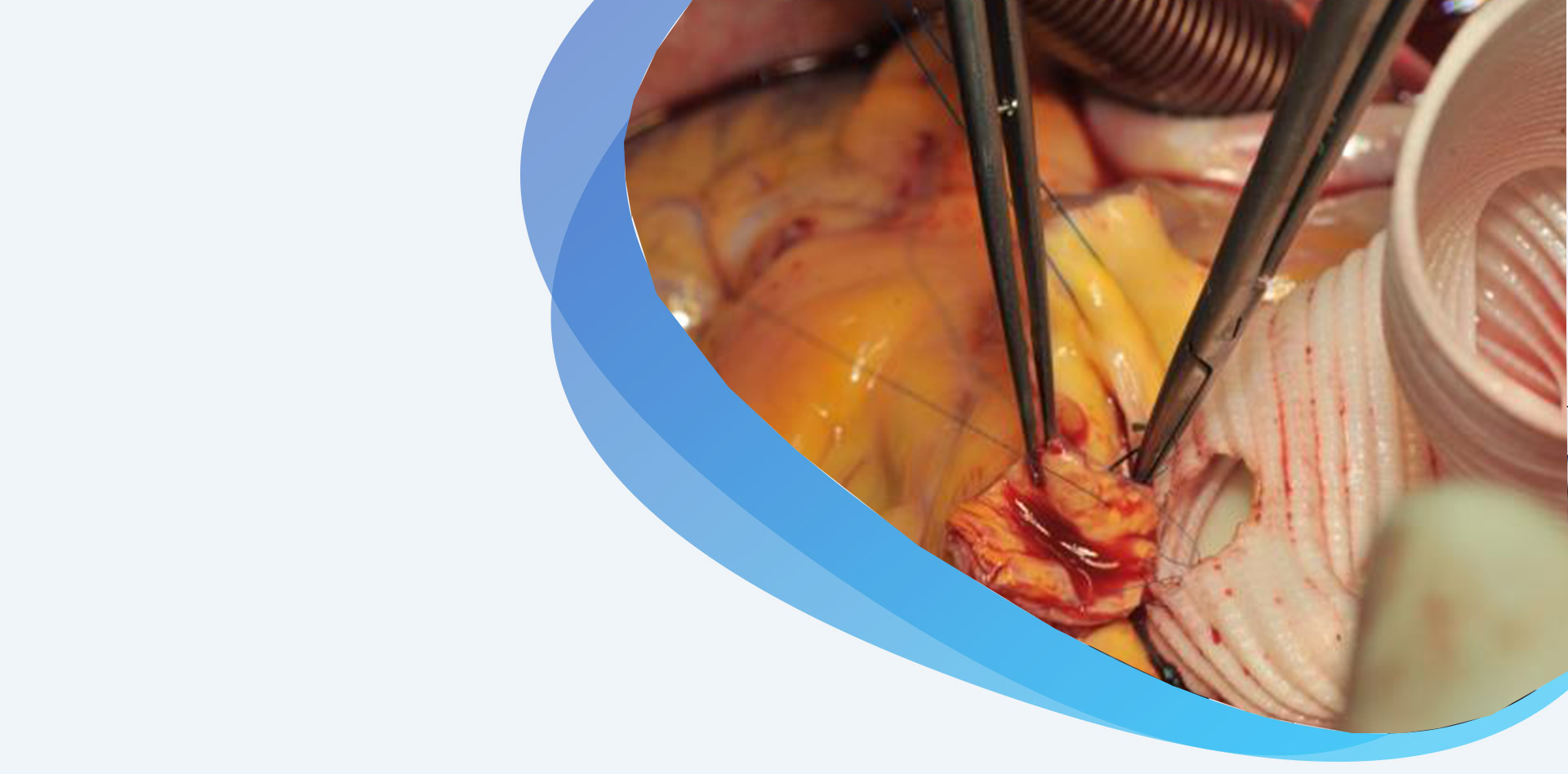
OPEN AORTIC RECONSTRUCTION
For about 30–40% of patients with an aortic dissection, over time, the aortic wall will dilate and form an aneurysm. When such an aneurysm grows to more than 6 cm in diameter, it will likely need repair through open aortic reconstruction. Careful assessment of your health condition is required before considering this extensive procedure. The goal is to completely remove the aneurysm—or, in higher-risk cases to remove the most serious portions.
- You are given general anesthesia.
- Once you are comfortable, you will be positioned so that you are lying on your right side. An incision is made along your left side that can extend from your shoulder blades to below your belly button.
- Your ribs are spread. Then, your vascular surgeon moves aside multiple organs (lungs, colon, kidney, spleen, pancreas, stomach) in order to reach the part of your aorta that needs to be fixed.
- Once the aorta is accessible, medication is given to thin your blood and your blood pressure is monitored.
- For your safety and to protect the spinal cord, kidneys and abdominal organs, a bypass circuit removes blood from the left side of the heart and pumps it into the legs and organs from below. This often requires another incision at the top of your leg.
- The aorta is clamped and repaired in segments. Then, major branches of the arteries that feed the abdominal organs and kidneys are clamped and repaired. The aorta below the kidney arteries is repaired last. Dissected portions of the aorta are replaced with cloth tubes that are sewn to the open ends of the vessel.
- The branches of the aorta that are involved in the repair may need to be replaced with smaller grafts or tubes. Smaller branches that are not essential may be over-sewn.
- Once all the necessary work is complete, blood thinner medication is reversed and the bypass circuit is removed. Your organs are checked and wounds are closed.